Endodontics Notes
*Cardial sign of inflammation & their causes:
Dolor = pain
Calor = heat
Tumor = swelling
Rabor = redness
Functionalsia = loss of function
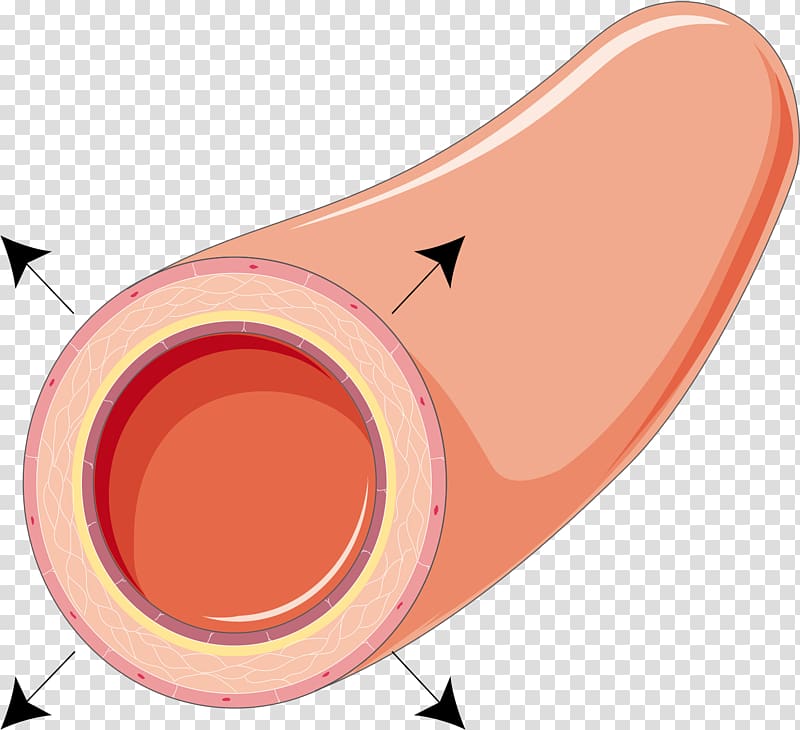
*First is vasodilation followed by vasoconstriction (anterior constriction); the sequence:
↑ blood flow
↑ vascular permeability
Enema / Exaduation
Escape of Leukocytes of sites of injury
necrosis
*Types of inflammation:
1. Chronic : long - Macrophages
2. Acute : suddenly - Neutophils
*Causes of pulpal inflammation:
1.Bacterial (most common cause)
2.Physical
3.Chemical
4.Idiopathic
1. Bacterial (mostly streptococcus mutans)
At Coronal (crown) & Radical (root) cause caries which leads to :
Fracture (complete or incomplete)
Non-fracture trauma (weakness due to pathologic)
once there is caries or fracture on crown which provide an opening or passage for bacteria to reach the apex & by disturbuting of infection cause widdening of periodomtal space & breakage of lamina dure & formation of sinus tract & in advance result toinflammation at lymph nodes:
Parotid gland = stensen's duct
Sublingual gland = Bartholin's duct
Submandibular gland = Wharton's duct
At Anomalous tract :
Tubercle or protuberance from the involved surface thats shows extra bump or cusp.
originates from the central groove or lingual ridge.
Dens invaginatus : incisor, most common is max lateral.
Dens envaginatus : Premolars & molars, most common is mandibular premolars.

At Radiation
Retrogenic infection through:
Periodontal inflammtion & calcular deposite cause 1.periodontal disease(gum recession) 2.periodontal pocket 3.periodontal abscess
Blood cause hematogenic (pertaining to the formation of blood or blood cells).
Saliva cause periodontal cancer by radiotion therapy.
bacteria has 2 way to reach apex: 1.pulp 2.periodontal ligument
2. Physical
Acute:
Sudden Fracture by 1.coronal 2. radiation
Vascular stasis during correction of orthodontic problem by forces that apply to the tooth.
Luxation (labial/buccal or lingual movement) & Avulsion (tooth suddenly lock out of socket)
Chronic:
Adolescent
Female Bruxism that leads to 1.Abrasion 2.Malocclusion 3.TMJ problem 4.Truma to periodontium 5.Pulp exposure
Attrition (physiological) /Abrasion (mechanical)
Erosion (chemical)
3. Chemical
Filiing material
cement:
IRM (Internative & Restorative material; Disadvantages is Expensive)
GIC (Flouride release that stop formation of caries)
Zinc Oxide Eugenol (Temporary cement that Promote tertiary dentin)
Polycarboxylate (True adhesion to tooth structure as a base or lutting cement when the cavity preparation is close to the pulp;The powder is zinc oxide & liquid is polyacrylic acid or a copolymer of that acid; Disadvantages are low tensile strength & no fluoride release & intraoral solubility)
Zinc phosphate (Never use in vital teeth because it contain acid & can irrigant the pulp)
Plastic:
Polymeric resins (use in restoring & replacing tooth structure or missing teeth that can be bonded with other resins or directly to tooth structure or to other restorative materials such as amalgam; Polymer is the liquid & Monomer is powder. Examples: Self cure resin & Heat cure resin)
Composite resin resotorative fillings (Because of the resin mimics has the appearance of natural teeth that also known as “white fillings” or “tooth-colored fillings")
Etching agent:
Removes smear layer & wet of the enamel to promote adhesion. 35% phosphoric acid for 15 seconds & wash well the tooth with water & dry after use
Cavity liners:
Cavity warnish for Amg
Bonding agent for composite
curing times is 20 sec
Alcohol/ether:
Cavity base that provides protection
Calcium hydeoxide (Dycal)
GIC type I (Luting cement for cementation of crown & bridges), type II (Restorative)
Disinfectant
AgNo3 (silver nitrate)
Phenol (using during pulpotomy)
NaFl (sodium fluorescein)
4. Iatrogenic
Cause by dentist druring:
Cavity prepration by Expose the pulp.
Restoration by wrong pack (No space between filling material).
Intentional extripation (ریشه کنی و نابئدی عمدی) by Exposing pulp tissue.
Orthodontic movement by forces that apply to the tooth.
Periodontal curettage by Severe mobility of tooth
Electrosurgery by Laser burns
Periapical curettage
Osteotomy by Cutting the bone.
Intubation by strike the teeth as it's rapidly and forcefully passed through the mouth and cause chipped teeth.

*Idiopathic - None cause:
Aging
Internal resorption

External reorption
Hypophosphatasia
Effect bone formation & disturbe mineralization
Sickle cell anemia
Hematogenic disease that decrease RBC so ↑ risk of infection.
*Pathogenesis:
1st ↓dentin permeability that leads to dentin sclerosis (hardening of dentin)
2nd formation of new dentin (secondary dentin)
3rd inflammatory & immune reaction (hyperemia) that leads to pulpitis then necrosis.
*Disease of the pulp :
1. Hyperemia
Physiologic term for inflammation.
↑ blood flow of pulp tissue.
Different with pulpitis.
Significance is 1st sign of pulp in stress.
Because of presence of causes (bacteria, trauma,...) that leads to Hypercemia (vasodilation followed by vasoconstriction) which finally result to Pulpitis.
2. Pulpitis
inflammation of pulp can be:
Acute/Chronic
Partial(some part of pulp expose) / Total (all part of pulp expose)
Infected (pus/abscess) / Sterile (no pus)
*Types of Pulpitis:
Inflammatory (Reversible & Irreversible)
Pulp Degeneration (calcific & Atrophic & Fibrous & Pulpartifacts & Tumors)
Necrosis
Inflammatory
Reversible
Mild to moderate inflammation of pulp because of noxious stimuli.
Px complain of pain that produced by thermal (hot & cold) stimuli.
Capable to retaining to uninflamed state by removal of stimuli.
Pain of brief duration produced by thermal stimuli.
Pain subside as soon as stimuli removed.
Sharp pain for few second or moment. (dentinal tubules is exposed)
Symptomes by cold food or cold air.
No accur spontaneously, its reactive.
No continue to accour when cause removed.
Thernal response are momentary, quick, sharp, hypersensitive response, subsides as soon as stimulus removed.
Percussion & Palpation is Negative.
in X-ray :
Caries not reach the pulp. (only in enamel or dentin)
No radiolucency at apex.
No widdening of periodontal space
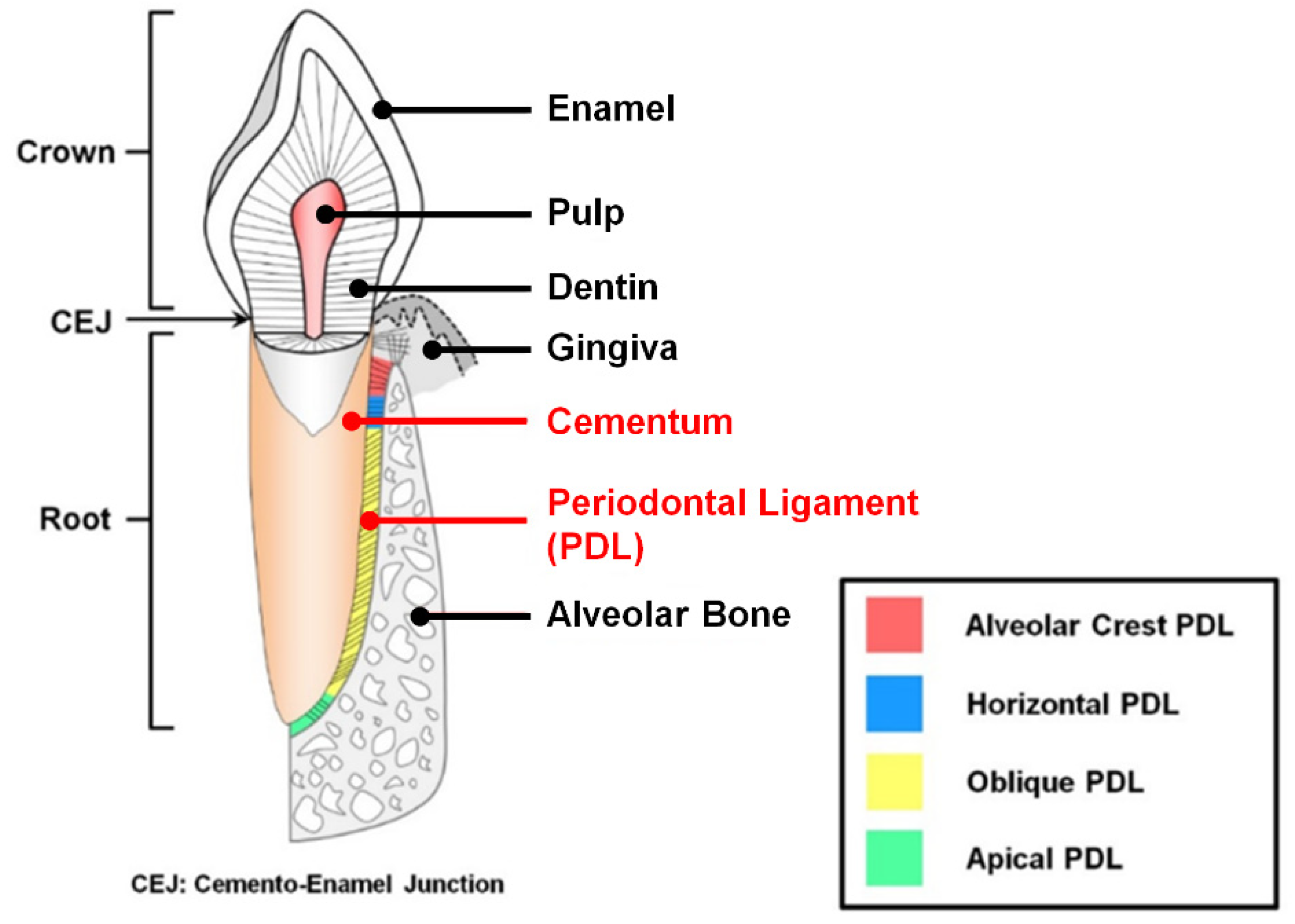
Lamina dura is intact - continious & radiopaque (lamina dura is thin bone occupize periodontal space but if there is break ,No contact)
Tx of reversible:
Early detectable & removal of cause.
Retreatment of cure.
prepare wet cavity & proper utilization chemical drug & restorative procedure.
Never desicate dentin during restorative procedure.
Outcome of treated reversible:
Favorable if irritant is removed early enough; if not detectable & treate on time, will continue & develop into irreversible.
Irreversible
Persistant inflammatory condition of pulp cause by Noxious stimulus.
Can be Symptomatic (pain) or Asymptomatic (no pain)
Can be Acute or Chronic.
Can be with Pus (infected) or No pus (sterile)
Progression of reversible pulpitis.
Pain caused by hot/cold stimulus.
Pain man accour spontaneously.
Pain persist for several min to hour.
Lingering after removal of thermal stimuli (Can ot go back to normal)
Hemorrhage & pain during probing.
In X-ray:
Deep cavity extending to pulp or decay under filling.
Caries exposed pulp or envolved surface of pulp.
Tx irreversible:
Emeregency tx is pulpectomy & placing material such as Formocresol (has too much formalin cause bone resoption)
Root canal tx
Extracted if its not restorable
Outcome of treated irreversible:
Favorable after proper endodontic procedure is done with proper restoration of tooth; if not detectable & treate on time, will continue & develop into necrosis.
Types of irreversible:
1. Acute
Short duration
Abnormally response tp cold/heat
Caries:
Smooth surface (labial, buccal, lingual, proximal)
Pit & Fissure&occlusal (lingual pit of max 1st molar, Buccal pit of mand molar, incisors)
Radiographic:
Deep caries with apparent pulpal exposure, extensive restoration
Theckening of periodontal space (advance stage)
Symptomatic:
Moderate-severe spomtaneous(accour naturally)
Inter mittent(on&off) or continous, sharp, dull
Radiating(not local,can go to neck) or Reffered(can not determined location), difficult to localize.
Intense pulsating type which becomes intermittent & throbbing
Contious for long period & worse when heat is applied
Pain relieved by application of heat/cold
Affect by postiral change(at night, sleep); Sleep with elevated head(seatin position)
Types of acute:
Suparative pulpitis presence of pus
Serous Pulpitis Extensive carise with No pulp expusure; Mild pain & increase sensivity during hot/cold test, sprecially hot test & negative to percussion
2. Chronic:
Asympotomatic
With pulp exposure
Hyperplastic pulpitis
Internal resorption
Types of chronic:
Chronic Close pulpitis No gross cavity & slowing advamcing caries
Chronic open pulpitis Big caries involvement
1. Ulcerative
expose the pulp & may favorable if symptomes relieved
2. Hyperplastic
Other name is pulp polyp
Chronic proliferative pulpitis, productive inflammation(hyperplasia) of pulp to extensive caries exposure of young pulp.
Characterized by development of granulation tissure that covered with epithelium; in otherword Granuloma with stratified squamous epithelium lined with polymorphous cell.
Clinical appearance is Fleshy reddish pulp that filled pulp chamber.
Resulting from long standing low grade irritation of pulp.
In young px & adult, no more above 50 y.o
Pain is not common unless disterbuted, painfull during presence of food & sensitive to hot/cold.
Tx is cut the pulp with spoonshape & excavation then RCT.
Outcome is favorable after endo tx or resto & can be unfavorable if left withouy tx.
X-ray of pulp polyp shows big radiolucency with direct access to pulp chamber.

*Pulp inflammation overview
1. pulp hyperemia
If does not treat will lead to Reveressible
2. Reversible pulpitis
If does not treat will lead to Irreveressible
3. Irreversible pulpitis
3.1. Actue Irreversible pulpitis
3.1.a. Acute Suparative pulpitis
3.1.b. Acute Serous pulpitis
3.2. Chronic Iireversible Pulpitis
3.2.a. Chronic Close pulpitis
3.2.a.b. Chronic Open Pulpitis
3.2.a.b.a. Chronic ulcerative Open Pulpitis
3.2.a.b.b. Chronic huperplastic Open Pulpitis
If does not treat will lead to Necrosis
4. Necrosis
4.1. Liquifactive necrotic pulp
4.2. Coagulative necrotic pulp
4.2.a. Caseation Coagulative necrotic pulp
Reversible | Irreversible |
Pain transient(short duration) & lasting in matter of second | Pain Continue after removal of stimulus & lasting for several month or longer |
Percussion negative | Percussion positive |
Mobility no | Mobility May or may not |
Sensitive cold | Sensitive hot/cold & sweet |
Necrosis
Common condition affecting tooth which pulp killed by Acute or Chronic inflammation.
History of pain that disappear.
Pulp extripation on tooth extraction is necessary.
Pulp Death that cause reduction of pain of tooth because all the tooth's nerves are in pulp, by death of pulp the px can feel the pain any more
Death of pulp can be partial or total.
sequel of inflammation of pulp following a traumatic injury:
1. Pulp is destroyed before inflammatory reaction takes place.
2. Ischemic infarction causing Dry-gangreous necrotic pulp whicj is blackage or bluish discoloration is most common cause by trauma.
3. Liquifactive, proleolytic enzyme convert pulp tissue into softtened mass that results liquid amorphous debris.
3. Coagulative necrotic, soluble portion of tissue is precipitated or converted into solid material.
4. Caseation is form of Coagulative necrotic, tissue converted to chessy mass consisting chiefly of Coagulated protein, fat, water.
End product of pulp decomposition is Hydrogen sulfide, Ammunis, Fleshy substance, Indican, Ptomaines, water, carbon dioxide.
Intermediate products contribute to unpleasant odor emanting from root of canal.
*Periapical Abscess
Result of decay & infection extending into pulp of tooth.
Break in periodontal ligument provide passage of bacteria toward the apex.
pain is severe, persistant, throbbing.
Tooth is tender to touch if not treted pus.
Tx:
Incision-dranaige of pus & Antibiotic therapy (Amoxicillin 500mg, Dispence # of antibiotic with type of anitbiotic either capsule or tablet, instruction take one capsule 3 times aday)
Root canal therapy
Extraction
*Periapical Granuloma:
Other name is Acute Periodontitis.
One of the most common sequel of pulpitis
Localized mass of chronic granulation tissue formed due to infection.
Hyperemia, Edeme, Inflammation of apical periodontal ligument.
X-ray:
Thickening of periodontal space
Root canal at apex is circumscribed.
*Osteomyelitis:
Inflammation of bone & bone marrow
Result of Odontogenic infection that develops to the Jaw.
Reference:
Lecture of Dr annalie De Lemos at national university college of dentistry-manila philippines
برچسبها: Endodonthics
