تشخیص اندو - پریو
کلاً ۵ نوع بیماری دارد:
- اندو اولیه
- پریو اولیه
- اندو اولیه پریو ثانویه
- پریو اولیه اندو ثانویه
- ترکیبی حقیقی اندو پریو
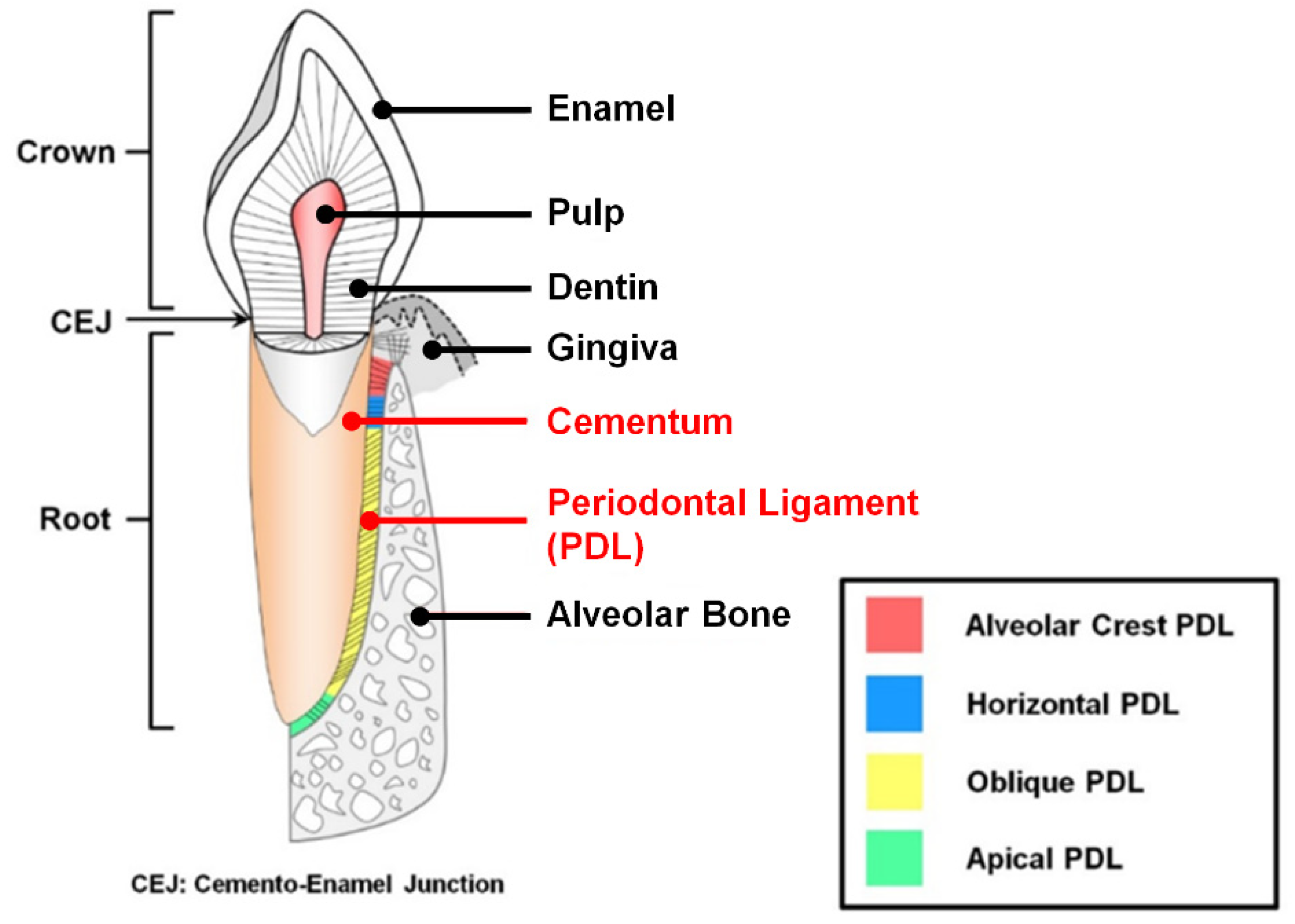
عفونت از دو طریق میتواند خود را به اپکس برساند : پالپ و PDL
اگر شروع عفونت از دندان باشد، کلمه ی اندو اولیه بکار میبریم یعنی اول اندو درگیر شده است.
اگر شروع عفونت از پریوونتشیوم باشد، کلمه ی پریو اولیه بکار میبریم یعنی اول پریو درگیر شده است.
دندان و پریودونتشوم توسط کانال های جانبی با هم در ارتباطند پس اگر عفونت از دندان شروع شود میتواند گسترش یابد و پریودونتشویم را هم درگیر کند که میگوییم اندو اولیه پریو ثانویه .
و بر عکس اگر از پریو شروع شود و بتواند گسترش یابد و اندو را هم درگیر کند که میگوییم پریو اولیه اندو ثانویه.
بطور خلاصه:
عفونت از دندان شروع شده و محدود به آن هم هست و پریودونتشیوم را درگیر نکرده: اندو اولیه
عفونت از دندان شروع شده و پریودونتشیوم را درگیر کرده: اندو اولیه پریو ثانویه
عفونت از پریودونتشیوم شروع شده و محدود به آن هم هست و دندان را درگیر نکرده: پریو اولیه
عفونت از پریودونتشیوم شروع شده و دندان را درگیر کرده: پریو اولیه اندو ثانویه
در شرح حال بیمار بدنبال کلماتِ کلیدی باشید که نشانگر یک تشخیص بخصوص است. در واقع این کلماتِ کلیدی مثل قفل و کلید برای تشخیصِ خود هستند؛ در جدول زیر برای هر بیماری، ویژگی اش آورده شده و ویژگی کلیدی آن قرمز رنگ شده است.
| اندو اولیه | پریو اولیه | اندو اولیه پریو ثانویه | پریو اولیه اندو ثانویه | ترکیبی حقیقی اندو پریو |
پالپ نکروز پاکتِ عمیق ِمنفردِ باریکِ بدونِ عرض سینوس ترکت باز شده به PDL عریض شدن فضای PDL رادیولوسنسی فضای استخوانی از اپکس به سرویکال رادیولوسنی فورکا از دست رفتن استخوان کرست ریج دورتادور اپکس سالکوس لثه سالم
| تحلیل عمودی/زاویه دار از سرویکال به اپکس ژنرالیزه فقدان پلیتِ باکال و لینگوال یا هردو پالپ زنده پاکت عمیقِ عریض تجمع پلاک و جرم افزایش عرضِ پاکت
| پلاک در مارژین لثه ای سینوس ترکت = پریودنتیت مارژینال عریض شدن PDL از اپکس تا سرویکال پاکت منفرد عریض تا اپکس تورم اگزودای چرک آبسه پریودنتال دردناک تشکیل پاکت لق شدن خونریزی و چرک حین BOP رادیولوسنسی عمیق در فورکا با گسترش تا اپکس | حلیل عمودی/زاویه دار از سرویکال به اپکس ضایعه ی پری اپیکال مجزا دندان اول ملتهب بوده پس درد داشته اما بعد نکروز شده و الان بدون درد ست پریودنتال ژنرالیزه پاکت عریض تا اپکس پالپ نکروز تحلیل نیمی از ارتفاعِ استخوانِ احاطه کننده ی ریشه تاج سالم و دست نخورده با پالپ نکروز اکسپوژر کانال های جانبی | از دست رفتن وسیع اتصالات پالپ نکروز پاکت پهن مخروطی ضایعه ی محدب تحلیل عمودی استخوان پاکت مخروطی دارای نقیصه ای که تا اپکس پروب میشود |
⚠️ نکات:
- در تمامی بیماری ها پالپ نکروز است به جز پریو اولیه
- پالپ زنده = پریو اولیه
- رادیو لوسنسی از اپکس به سرویکال = اندو اولیه
- رادیولوسنسی از سرویکال به اپکس= پریو اولیه
- پاکتِ کَمَر باریک = اندو اولیه
- پاکتِ کَمَر پهن = پریو اولیه
- چرک = اندو اولیه پریو ثانویه
- رادیولوسنسی فورکا = اندو اولیه
مثال:
- خانمی ۲۸ ساله برای معاینه ی روتین به دندانپزشکی مراجعه کرده است، در بررسی رادیوگرافی دندان ۵ پایین چپِ بیمار مشکوک بود پس تست های حیاتی گرفته شد و دندان به تمامی تست ها پاسخ نداد و یک پاکت عمیقِ باریک یافت شد اما سولکوس لثه سالم است؛ تشخیص؟
پاسخ : اندو اولیه
توضیح: پاکت عمیقِ باریک نشانگر اندو اولیه است یعنی شروع بیماری از دندان بوده پس تشخیص اندو اولیه یا اندو اولیه پریو ثانویه است. در ادامه سوال میبینیم به لثه ی سالم اشاره شده پس بافت پریودونتشیوم هنوز درگیر نشده و محدود به دندان است پس گزینه ی اندو اولیه پریو ثانویه حذف میشود و جواب اندو اولیه است.
- آقایی ۳۸ ساله با درد و تورم مراجعه کرده است و در معاینه کلینیکی چرک مشاهده شده است و دندان به تست های حیاطی پاسخ نمیدهد و یک پاکت منفرد عریض تا اپکس هم مشاهده میشود؛ تشخیص؟
پاسخ: اندو اولیه پریو ثانویه
توضیح: چرک = اندو اولیه پریو ثانویه
برچسبها: Endodonthics
Endodontics Notes
*Cardial sign of inflammation & their causes:
Dolor = pain
Calor = heat
Tumor = swelling
Rabor = redness
Functionalsia = loss of function
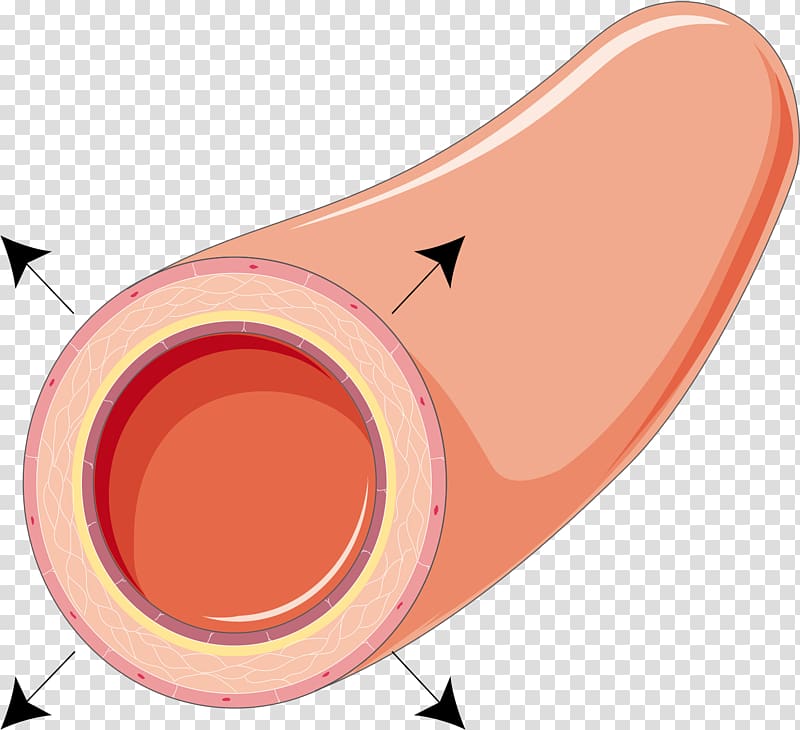
*First is vasodilation followed by vasoconstriction (anterior constriction); the sequence:
↑ blood flow
↑ vascular permeability
Enema / Exaduation
Escape of Leukocytes of sites of injury
necrosis
*Types of inflammation:
1. Chronic : long - Macrophages
2. Acute : suddenly - Neutophils
*Causes of pulpal inflammation:
1.Bacterial (most common cause)
2.Physical
3.Chemical
4.Idiopathic
1. Bacterial (mostly streptococcus mutans)
At Coronal (crown) & Radical (root) cause caries which leads to :
Fracture (complete or incomplete)
Non-fracture trauma (weakness due to pathologic)
once there is caries or fracture on crown which provide an opening or passage for bacteria to reach the apex & by disturbuting of infection cause widdening of periodomtal space & breakage of lamina dure & formation of sinus tract & in advance result toinflammation at lymph nodes:
Parotid gland = stensen's duct
Sublingual gland = Bartholin's duct
Submandibular gland = Wharton's duct
At Anomalous tract :
Tubercle or protuberance from the involved surface thats shows extra bump or cusp.
originates from the central groove or lingual ridge.
Dens invaginatus : incisor, most common is max lateral.
Dens envaginatus : Premolars & molars, most common is mandibular premolars.

At Radiation
Retrogenic infection through:
Periodontal inflammtion & calcular deposite cause 1.periodontal disease(gum recession) 2.periodontal pocket 3.periodontal abscess
Blood cause hematogenic (pertaining to the formation of blood or blood cells).
Saliva cause periodontal cancer by radiotion therapy.
bacteria has 2 way to reach apex: 1.pulp 2.periodontal ligument
2. Physical
Acute:
Sudden Fracture by 1.coronal 2. radiation
Vascular stasis during correction of orthodontic problem by forces that apply to the tooth.
Luxation (labial/buccal or lingual movement) & Avulsion (tooth suddenly lock out of socket)
Chronic:
Adolescent
Female Bruxism that leads to 1.Abrasion 2.Malocclusion 3.TMJ problem 4.Truma to periodontium 5.Pulp exposure
Attrition (physiological) /Abrasion (mechanical)
Erosion (chemical)
3. Chemical
Filiing material
cement:
IRM (Internative & Restorative material; Disadvantages is Expensive)
GIC (Flouride release that stop formation of caries)
Zinc Oxide Eugenol (Temporary cement that Promote tertiary dentin)
Polycarboxylate (True adhesion to tooth structure as a base or lutting cement when the cavity preparation is close to the pulp;The powder is zinc oxide & liquid is polyacrylic acid or a copolymer of that acid; Disadvantages are low tensile strength & no fluoride release & intraoral solubility)
Zinc phosphate (Never use in vital teeth because it contain acid & can irrigant the pulp)
Plastic:
Polymeric resins (use in restoring & replacing tooth structure or missing teeth that can be bonded with other resins or directly to tooth structure or to other restorative materials such as amalgam; Polymer is the liquid & Monomer is powder. Examples: Self cure resin & Heat cure resin)
Composite resin resotorative fillings (Because of the resin mimics has the appearance of natural teeth that also known as “white fillings” or “tooth-colored fillings")
Etching agent:
Removes smear layer & wet of the enamel to promote adhesion. 35% phosphoric acid for 15 seconds & wash well the tooth with water & dry after use
Cavity liners:
Cavity warnish for Amg
Bonding agent for composite
curing times is 20 sec
Alcohol/ether:
Cavity base that provides protection
Calcium hydeoxide (Dycal)
GIC type I (Luting cement for cementation of crown & bridges), type II (Restorative)
Disinfectant
AgNo3 (silver nitrate)
Phenol (using during pulpotomy)
NaFl (sodium fluorescein)
4. Iatrogenic
Cause by dentist druring:
Cavity prepration by Expose the pulp.
Restoration by wrong pack (No space between filling material).
Intentional extripation (ریشه کنی و نابئدی عمدی) by Exposing pulp tissue.
Orthodontic movement by forces that apply to the tooth.
Periodontal curettage by Severe mobility of tooth
Electrosurgery by Laser burns
Periapical curettage
Osteotomy by Cutting the bone.
Intubation by strike the teeth as it's rapidly and forcefully passed through the mouth and cause chipped teeth.

*Idiopathic - None cause:
Aging
Internal resorption

External reorption
Hypophosphatasia
Effect bone formation & disturbe mineralization
Sickle cell anemia
Hematogenic disease that decrease RBC so ↑ risk of infection.
*Pathogenesis:
1st ↓dentin permeability that leads to dentin sclerosis (hardening of dentin)
2nd formation of new dentin (secondary dentin)
3rd inflammatory & immune reaction (hyperemia) that leads to pulpitis then necrosis.
*Disease of the pulp :
1. Hyperemia
Physiologic term for inflammation.
↑ blood flow of pulp tissue.
Different with pulpitis.
Significance is 1st sign of pulp in stress.
Because of presence of causes (bacteria, trauma,...) that leads to Hypercemia (vasodilation followed by vasoconstriction) which finally result to Pulpitis.
2. Pulpitis
inflammation of pulp can be:
Acute/Chronic
Partial(some part of pulp expose) / Total (all part of pulp expose)
Infected (pus/abscess) / Sterile (no pus)
*Types of Pulpitis:
Inflammatory (Reversible & Irreversible)
Pulp Degeneration (calcific & Atrophic & Fibrous & Pulpartifacts & Tumors)
Necrosis
Inflammatory
Reversible
Mild to moderate inflammation of pulp because of noxious stimuli.
Px complain of pain that produced by thermal (hot & cold) stimuli.
Capable to retaining to uninflamed state by removal of stimuli.
Pain of brief duration produced by thermal stimuli.
Pain subside as soon as stimuli removed.
Sharp pain for few second or moment. (dentinal tubules is exposed)
Symptomes by cold food or cold air.
No accur spontaneously, its reactive.
No continue to accour when cause removed.
Thernal response are momentary, quick, sharp, hypersensitive response, subsides as soon as stimulus removed.
Percussion & Palpation is Negative.
in X-ray :
Caries not reach the pulp. (only in enamel or dentin)
No radiolucency at apex.
No widdening of periodontal space
Lamina dura is intact - continious & radiopaque (lamina dura is thin bone occupize periodontal space but if there is break ,No contact)
Tx of reversible:
Early detectable & removal of cause.
Retreatment of cure.
prepare wet cavity & proper utilization chemical drug & restorative procedure.
Never desicate dentin during restorative procedure.
Outcome of treated reversible:
Favorable if irritant is removed early enough; if not detectable & treate on time, will continue & develop into irreversible.
Irreversible
Persistant inflammatory condition of pulp cause by Noxious stimulus.
Can be Symptomatic (pain) or Asymptomatic (no pain)
Can be Acute or Chronic.
Can be with Pus (infected) or No pus (sterile)
Progression of reversible pulpitis.
Pain caused by hot/cold stimulus.
Pain man accour spontaneously.
Pain persist for several min to hour.
Lingering after removal of thermal stimuli (Can ot go back to normal)
Hemorrhage & pain during probing.
In X-ray:
Deep cavity extending to pulp or decay under filling.
Caries exposed pulp or envolved surface of pulp.
Tx irreversible:
Emeregency tx is pulpectomy & placing material such as Formocresol (has too much formalin cause bone resoption)
Root canal tx
Extracted if its not restorable
Outcome of treated irreversible:
Favorable after proper endodontic procedure is done with proper restoration of tooth; if not detectable & treate on time, will continue & develop into necrosis.
Types of irreversible:
1. Acute
Short duration
Abnormally response tp cold/heat
Caries:
Smooth surface (labial, buccal, lingual, proximal)
Pit & Fissure&occlusal (lingual pit of max 1st molar, Buccal pit of mand molar, incisors)
Radiographic:
Deep caries with apparent pulpal exposure, extensive restoration
Theckening of periodontal space (advance stage)
Symptomatic:
Moderate-severe spomtaneous(accour naturally)
Inter mittent(on&off) or continous, sharp, dull
Radiating(not local,can go to neck) or Reffered(can not determined location), difficult to localize.
Intense pulsating type which becomes intermittent & throbbing
Contious for long period & worse when heat is applied
Pain relieved by application of heat/cold
Affect by postiral change(at night, sleep); Sleep with elevated head(seatin position)
Types of acute:
Suparative pulpitis presence of pus
Serous Pulpitis Extensive carise with No pulp expusure; Mild pain & increase sensivity during hot/cold test, sprecially hot test & negative to percussion
2. Chronic:
Asympotomatic
With pulp exposure
Hyperplastic pulpitis
Internal resorption
Types of chronic:
Chronic Close pulpitis No gross cavity & slowing advamcing caries
Chronic open pulpitis Big caries involvement
1. Ulcerative
expose the pulp & may favorable if symptomes relieved
2. Hyperplastic
Other name is pulp polyp
Chronic proliferative pulpitis, productive inflammation(hyperplasia) of pulp to extensive caries exposure of young pulp.
Characterized by development of granulation tissure that covered with epithelium; in otherword Granuloma with stratified squamous epithelium lined with polymorphous cell.
Clinical appearance is Fleshy reddish pulp that filled pulp chamber.
Resulting from long standing low grade irritation of pulp.
In young px & adult, no more above 50 y.o
Pain is not common unless disterbuted, painfull during presence of food & sensitive to hot/cold.
Tx is cut the pulp with spoonshape & excavation then RCT.
Outcome is favorable after endo tx or resto & can be unfavorable if left withouy tx.
X-ray of pulp polyp shows big radiolucency with direct access to pulp chamber.

*Pulp inflammation overview
1. pulp hyperemia
If does not treat will lead to Reveressible
2. Reversible pulpitis
If does not treat will lead to Irreveressible
3. Irreversible pulpitis
3.1. Actue Irreversible pulpitis
3.1.a. Acute Suparative pulpitis
3.1.b. Acute Serous pulpitis
3.2. Chronic Iireversible Pulpitis
3.2.a. Chronic Close pulpitis
3.2.a.b. Chronic Open Pulpitis
3.2.a.b.a. Chronic ulcerative Open Pulpitis
3.2.a.b.b. Chronic huperplastic Open Pulpitis
If does not treat will lead to Necrosis
4. Necrosis
4.1. Liquifactive necrotic pulp
4.2. Coagulative necrotic pulp
4.2.a. Caseation Coagulative necrotic pulp
Reversible | Irreversible |
Pain transient(short duration) & lasting in matter of second | Pain Continue after removal of stimulus & lasting for several month or longer |
Percussion negative | Percussion positive |
Mobility no | Mobility May or may not |
Sensitive cold | Sensitive hot/cold & sweet |
Necrosis
Common condition affecting tooth which pulp killed by Acute or Chronic inflammation.
History of pain that disappear.
Pulp extripation on tooth extraction is necessary.
Pulp Death that cause reduction of pain of tooth because all the tooth's nerves are in pulp, by death of pulp the px can feel the pain any more
Death of pulp can be partial or total.
sequel of inflammation of pulp following a traumatic injury:
1. Pulp is destroyed before inflammatory reaction takes place.
2. Ischemic infarction causing Dry-gangreous necrotic pulp whicj is blackage or bluish discoloration is most common cause by trauma.
3. Liquifactive, proleolytic enzyme convert pulp tissue into softtened mass that results liquid amorphous debris.
3. Coagulative necrotic, soluble portion of tissue is precipitated or converted into solid material.
4. Caseation is form of Coagulative necrotic, tissue converted to chessy mass consisting chiefly of Coagulated protein, fat, water.
End product of pulp decomposition is Hydrogen sulfide, Ammunis, Fleshy substance, Indican, Ptomaines, water, carbon dioxide.
Intermediate products contribute to unpleasant odor emanting from root of canal.
*Periapical Abscess
Result of decay & infection extending into pulp of tooth.
Break in periodontal ligument provide passage of bacteria toward the apex.
pain is severe, persistant, throbbing.
Tooth is tender to touch if not treted pus.
Tx:
Incision-dranaige of pus & Antibiotic therapy (Amoxicillin 500mg, Dispence # of antibiotic with type of anitbiotic either capsule or tablet, instruction take one capsule 3 times aday)
Root canal therapy
Extraction
*Periapical Granuloma:
Other name is Acute Periodontitis.
One of the most common sequel of pulpitis
Localized mass of chronic granulation tissue formed due to infection.
Hyperemia, Edeme, Inflammation of apical periodontal ligument.
X-ray:
Thickening of periodontal space
Root canal at apex is circumscribed.
*Osteomyelitis:
Inflammation of bone & bone marrow
Result of Odontogenic infection that develops to the Jaw.
Reference:
Lecture of Dr annalie De Lemos at national university college of dentistry-manila philippines
برچسبها: Endodonthics
ENDODONTICS BASIC STEPS
A. case selection:
There are general criteria to approve a case for endo tx:
1. At least one third of the crown length must be intact after caries removal & carious involvement should not be located in the subgingival level.
2. Must have healthy ginigival & periodontal tissues.
3. Periapical lesion involvement should not be more than one third of the length of the root.
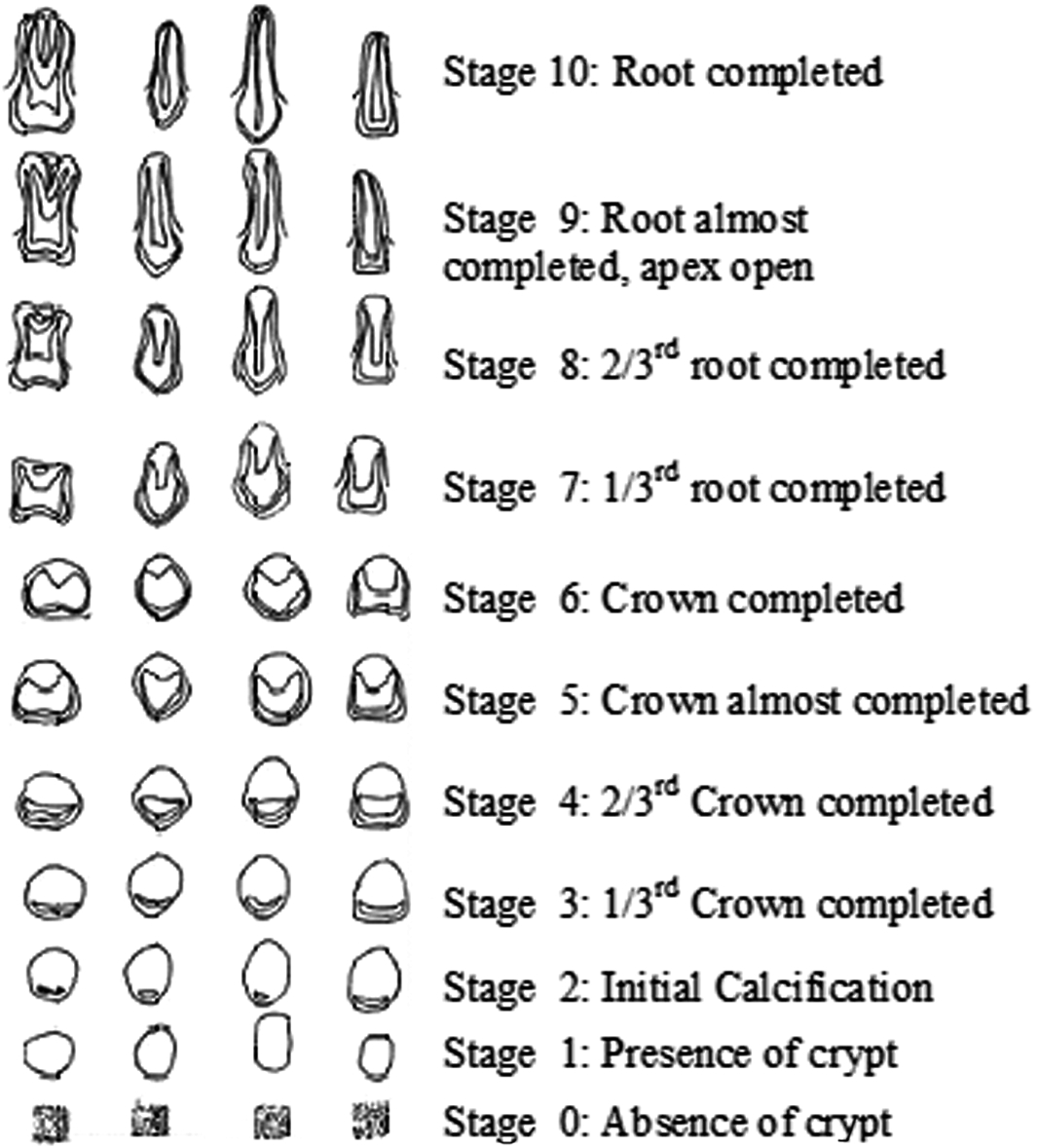
4. Must have complete development of the root apex (at least until nolla stage 9).
5. Tooth mobility must be limited to 2nd degree & should be restored after initial tx.
6. Must have NO radicular fracture in any form.
7. Restorability of the tooth must be considered after RCT ( final restoration).
8. Accessibility of the apical foramen trough the root canal should be considered & severity of curved canal.
9. General health of thre px should always be evaluated.
If the case Does not have this conditions, REFER to specialist ! Do not start what you can not finish.
B. Diagnosis
1. Clinical examination:
*Vitality test : for examination of tooth including thermal test( heat test & cold test) & EPT & cavity test ( last choice)
*Percussion :for examination of periodontium (specially periodontal ligument)
*Palpation : for examination of gingiva
2. Sign & Symptoms
3. Case history
4. Radiographic interpretation
* Summerized diagnosis:
1. Vital case :
*Reversible pulpitis (which can be tx by resto)
*Irreversible pulpitis-symptomatic or asymptomatic (needs endo tx)
2. Non- vital case:
*Necrosis ( needs endo tx)
*Acute/chronic priapical infection /apical periodontitis
*Acute/chronic periapical abscess- sinus tract / fistula ( once you have sinus tract, your diagnosis is CPI-chronic periapical infection for sure )
)
C. Radiographic interpretation:
1. The offending tooth must appear in the middle of radiograph & the entire length of the root & its periapical structure must be included.
2. Radiograph must be always clear
3. Clinician should be able to describe the following:
*Condition of the lamina dura
*Condition of the periodontal space
*Condition of the periapical structures
*For example:
At first we should start from UP to Down
#tooth 11 : crown is intact, caries found on the middle 3rd of crown at distal side & does not extent to pulp, one straight single rooth, lamina dura is intact, normal periodontal space, no radiolucency found at apex.
#tooth 12 : crown is intact, Big caries found on the middle 3rd of crown at both mesial & distal side but does not extent to pulp, one straight single rooth, breakage of lamina dura, widdening periodontal space, no radiolucency found at apex.
D. Caries removal:
Remove all the soft caries and be sure that only sound tissure are reamin to prevent RECURRENT CARIES. if the px has pain during caries removal apply anesthesia.

E. Anesthesia:
*After caries removal which may need anesthesia, for next step which is Access prepration you need anesthesia that usually for anterior tooth(upp & low) infiltration & for upp post infiltartion & for low post IAN Block are suffeciant.
*If the case is pulp necrosis usually you do not need anesthesia but if the px is not comfort and has pain due to rubber dam assembly , apply infiltartion to anesthestze sorrounding soft tissue or choose other method of isolation( like 1. rubber dam split which is rubber dam and floss only 2. cotton roll isolation).
F. Building up of walls:
*After caries removal if its neccessary we should build up of walls with composite to reach our specific design for our outline.
*To provide a proper seal for the canal during and after treatment.
*An speceific canal is the key to success of the treatment.
*Example of a case that after caries removal needs crown build up
G. Rubber dam isolation:
*To prevent accidental swallowing of any endodontic instrument by the px (most common purpose) & to provide proper visibility & to provide an aseptic environment during tx.
*The bow of the clamp should be at DISTAL side of the tooth .
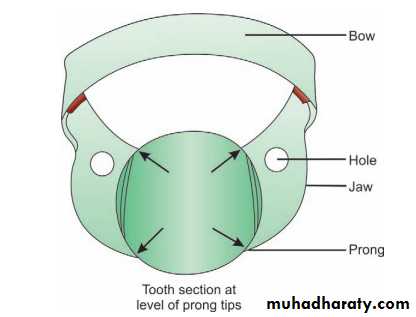
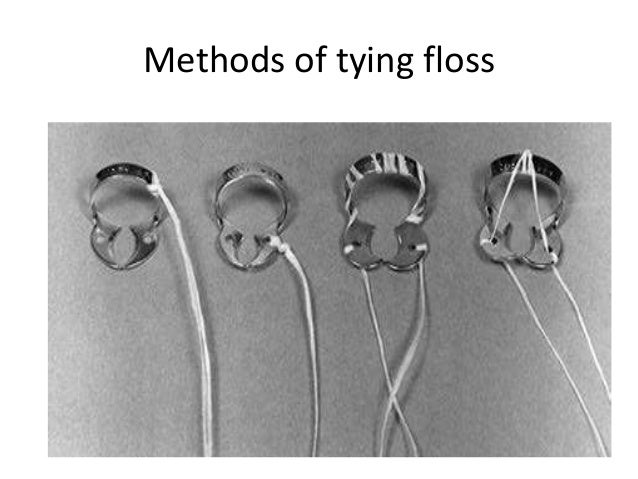
*Tie with Dental floss to avoid swallowing problem:
*use rubber dam sheet perforation template for better placement of rubber dam sheet on clamp base on offending tooth.

*Rubber dam used mostly in blue color and green color & clinician always use rubber dam :green size 6 by 6 medium size.
*clamp frame used to hold rubber dam away from px face and has plastic & metal.use plastic one to avoid any problem during taking x-ray.
*Example of acceptable Rubberdam isolation:

H. Access prepration:
1. The objectives of access prepration:
*maximum visibility - To locate and permit adequate access to the canals.
*Removal of caries, debris from the chamber and pulp horns.
*To achieve a staright-line access to the canal and to minimize curvature.
*Example of acceptable cavity access
2. steps in access prepration
*Proper outline form
*Unroofing
*Starigh line access
3. How?
*Use round 1/2 (Smal)l bur for initial access with 45 degree after 1st drop use 1/8 ( big) round bur with 90 degree for access and for unroofing use non end cutting & finishing Endo bur for refinement of walls.
I. pullp excavation / canal debridement:
*Use spoon shape excavator to remove pulp from pulp chamber
*Use barbed broach to remove pulp from root canals.

*Irrigant used in 1:9 dilution of 5.2% sodium hypochlorite & distilled water delivered into canal with a disposable syringe.
*scoop technique: bend the needle 90 degree by needle cover to avoid needle stick in canal during irrigation.
M. Root canal prepration:
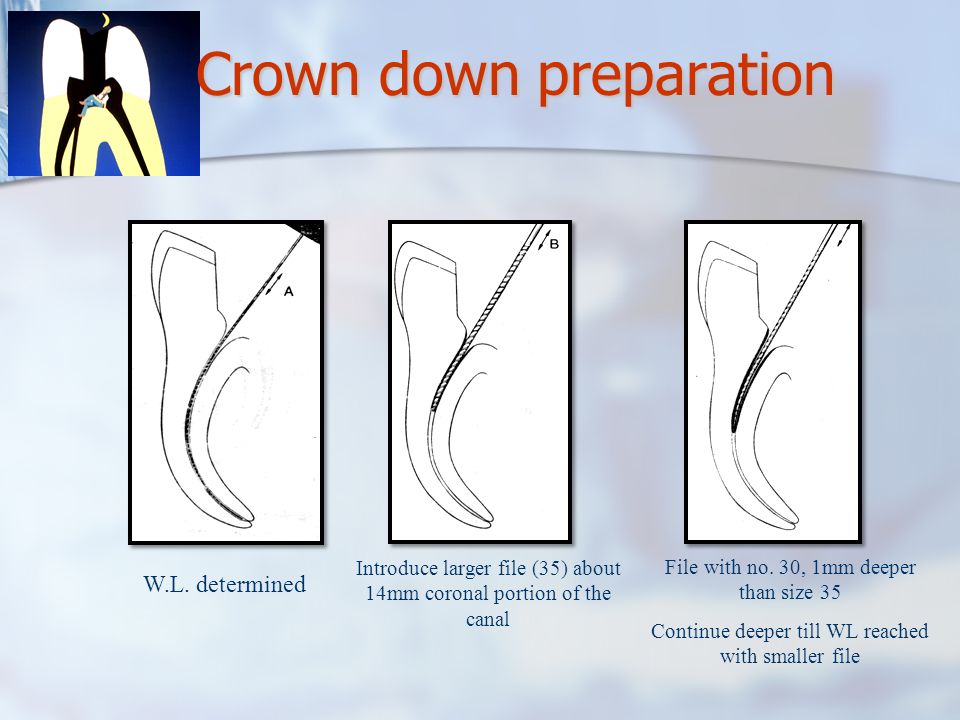
1. Crown down prepration
*To remove any constriction on the coronal 2/3rd of the canals &t o open the canal orifices.
*For example your MAF is 35 at 18 mm so your setp back sequence ganna be like this:
file size 50 at 15 mm
file size 45 at 16 mm
file size 40 at 17 mm
file size 35 at 18 mm
2. Working length determination
*To establish the lenghth of canal prepration & obturation, you should compute Tooth Lengh Image.
*Select the reference point that ususally for ant is IE (incisal edge) & for post is cusp or OE (occlusal edge).
*WL = TLI-Safe factor (TLI is tooth length image that is measured by ruler from radiographic image).
*SF:Safe factor is -2mm use to be sure the accuracy of measurement dute risk of forshortened error and avoid apical perforation.
*After computing TLI transfer it to IAF file (initial apical filing) with a stopper (stopper should rest at reference point) and take a radiograph. If you see your file is flush (no discrepency) so youR WL is correct=actual working length but if you see the file is short so you shoud add the difference(+discrepency)to your WL and get your actual working length and if you see your file is over you shouf minimize the difference from WL (-discrepency)to get actual working length. ( AWL: WL +/- Discrepency)
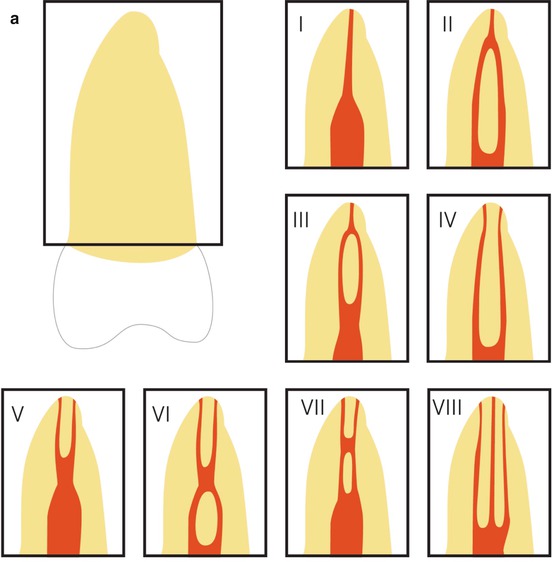
*Apical constriction: the smallest apical diameter and is located 0.5–1.5 mm inside the apical foramen & working lengh must be above of this area to prevent overextention & apical perforation.
*Example of acceptable WL

3. Apical prepration
1. Scouting : To evaluate the cross sectional diameter of a canal & to provide information as the whether the canal is open ,partially restricted , calcified, dilacerated, devided or ect.
2. Patency: Is established by using a #10 file by moving it gently in a push-pull motion until it easly moves into the pre-established working length ( to see if canal is open or no & this step is neccessery to avoid any fracture inside the canal )

*Start filing with IAP by using proper file size at working length.
3. Serial filling : Enlarge the apical 3rd of the canal up tp 3 size bigger from the IAF at working lenghth & the last file used during procedure will be MAF ( master apical file) for example:
IAF (file 20 at 18mm) 1. file 25 at 18mm 2. 30 file at 18mm 3. file 35 at 18mm (MAF)
*The minimum file size for MAF is 25 so for example if your IAF is #6 during serial filling you should enlarge the canal 5 times to reach #25 for your MAF(1.#8 2.#10 3.#15 4.#20 5.#25).
*Example of opening apical 3rd of canal by serial fillin
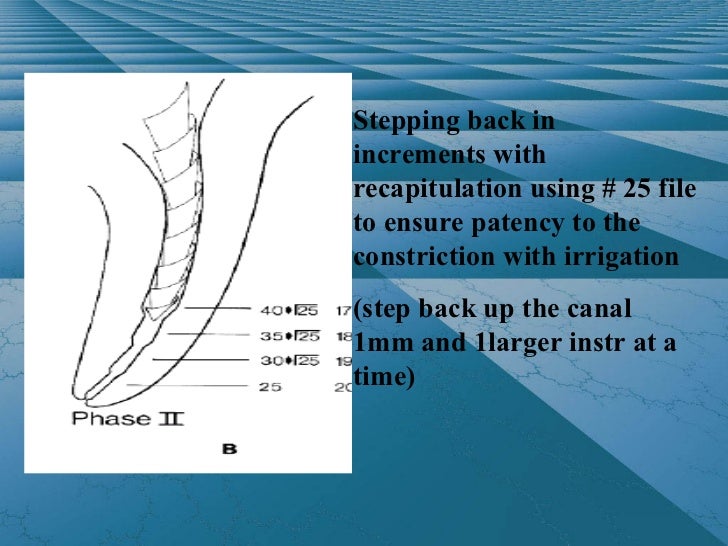
5. Step back: Enlarge the coronal portion of root by enlarging of MAF 3 times bigger.
*Every time that you enlarge the file, you have to minimize your working length 1mm & again go back to you MAF with original AWL and repeat it 3 times .
*You should finish the procedure with MAF at original AWL .for example:
MAF 35 at 18mm
file 40 at 17mm
MAF 35 at 18mm
file 45 at 16mm
MAF 35 at 18mm
file 50 at 15mm
MAF 35 at 18mm
*Example enlarging coronal portion of canal by step back
*In rotary all the steps are same & just needs to skip step back.
*For file sterilization use Glass bead for 15 sec.
*If you have difficulty to open the canal use occaliptus or orange oil (wet the files with oil then insert)
N. Circumferential filling:
*choose SRT(spreader test) file which is one size bigger than you MAF but -2MM shorter than MAF.
*Insert MAF &SRT together into the canal To Flare the canal.
*Example of placing SRT and MAF inside the canal.

P. Master cone:
*Use a gutta percha as same size & length with your MAF.
*After inserting the master cone at AWL , check with cotton plier for tugback = resistance .
*True tugback is as result of apical seal which is correct.
*Example of accepetd mastercone

*False tugback is a result of middlle 3rd bending which is not correct.
*Example of Fulse tugback
*For gutta percha sterilization : rinsed in isopropyl alcohol for 1min.
Q. Patient evaluation:
*If the case has radiolucency at apex or presence of sinus tract, its better to do endo tx in two visit.
*At 1st meeting exclusive for cleaning & shaping only & dismiss the px with putting a cotton pelet (can be wet by Eugenol for disinfectant puposes) and cover it with fermin & place composite as a temporary restoration & ask px to come back after 1 week.
*At 2nd meeting check the 7 sign then proceed to obturation:
1. No radiolucency at apex
2. No foul odor ( use paper point, insert it to canal and smell it)
3. No bleeding
4. No pain
5. Seal intact ( the temporary restoration& fermin & cotton shoul be in place otherwise you should repeat from serial filling cause we should be sure NO bacterias are inside the canal)
6. Dry canal
7. Negative culture test
R. obturation:
1. Place your spreader test at sealer ( low set IRM)
2. Insert the spreader test inside the canal & wet all the walls with IRM.
3. Place the master cone in sealer & insert it to canal at AWL.
4. Placr your spreader test at sealer & do lateral condensation technique.
5. Place one size smaller at 1mm shorter gutta percha in sealer & insert it to canal & do lateral condensation technique.
6. Repeat untill you reach #15 gutta percha & then just fill the rest with #15 & sealer.
*example of acceptable obturation

S. Obturation uncut:
*Before you cut the gutta perchas , be sure that your obturation has this conditions.
1. NO voids ( radiolucency that fount and obturation which can be passage of bacteria)
2. fully fill radiopaque that followed tooth walls & anatomy
3. No overextention
4. No Underextention
5. NO lefted canal
*In case that you need to repeat your obturation:
1. Use formaldehyde to soften & remove gutta pecha.
2. Irrigate the canal with irrigator and dry the canal with paper point.
3. Once you put your master cone in the canal to check tugback ,befiore you place it in sealer , rinse it in isopropyl alcohol for 1min to be sure no formaldehyde is attached to your master cone & your master cone is hard enough.
*Example of obturation with voids

T. Obturation cut:
*Cut the gutta percha 1mm beyond CEJ.
*Be sure during cutting with gutta percha remover is hot enough to avoild upward moving of gutta perchas and shortening of obturation.
*Example of acceptable obturation cut

W. Final restoration:
*After cutting gutta percha , clean the space well with cotton pelet & alcohol to be sure no sealer are intact with walls.
*Use GIC TYPE2 - RESTORATIVE to fill the space then place the composite.
*Because if your final restoration is composite, due to presence of Eugenol in IRM (sealer) that can cause oxidation & prevent composite polymirization so if the sealer come in contact with IRM, eugenol will prevent composite to set and we will have shrinkage of composite.
Reference:
Lecture of Dr annalie De Lemos at national university college of dentistry-manila philippines
برچسبها: Endodonthics
