WOUND REPAIR
Active TROMBIN cleaves FIBRINOGEN into FIBRIN, which polymerizes into a fibrin network (SCAB) sealing the wound
CAUSES OF TISSUE DAMAGE
Physical
Copromised blood flow
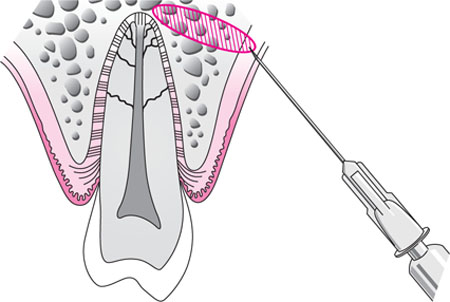
Crushing
Desiccation
Incision
Irradiation
Overcooling
Overheating
Chemical
Agent with unphysiologic PH
Agent with unphysiologic tonicity
Proteases
Vasoconstrictors
Thrombogenic agents
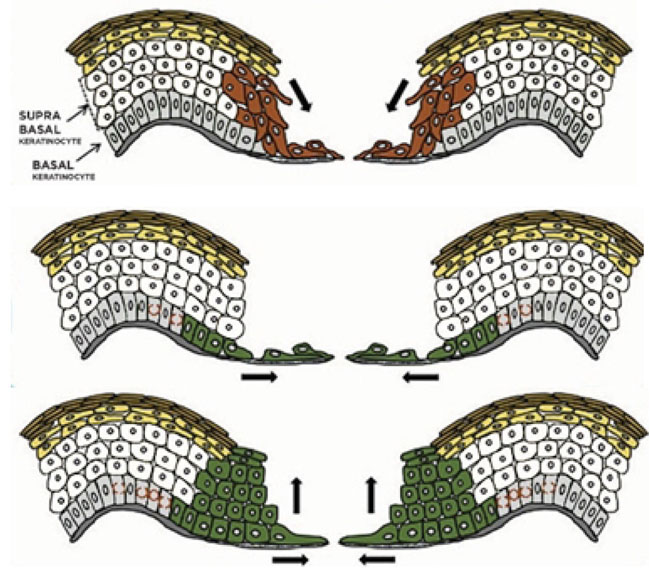
EPITHELIALIZATION
Injured epithelium has a genetically programmed regenerative ability that allows it to reestablish its integrity through proliferation, migration & a process known as contact inhibition
In general, any free edge of epithelium continues to migrate (by proliferation of germinal epithelial cells that advance the free edge forward) until it comes into contact with another free edge of epithelium, where it is signaled to stop growing laterally
Wounds in which only the surface epithelium is injured (e.g. abrasions) heal by proliferation of epithelium across the wound bed
Wounds in which the sub-epithelial tissue is also damaged proliferates across whatever vascularized tissue bed is available & stays under the portion of the superficial blood clot that desiccates (forms a scab) until it reaches another epithelial margin. Once the wound is fully epithelialized, the scab loosens and is dislodged
STAGES of WOUND HEALING
Inflammatory Stage
Fibroplastic Stage
Remodelling Stage
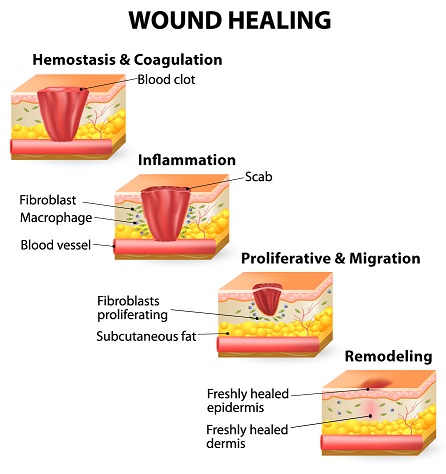
Inflammatory Stage
“Lag Phase” – the period where no significant gain in wound strength occurs.
Principal material holding together during this stage is fibrin.
Wound fills with clotted blood, inflammatory cells and plasma.
Adjacent tissue begins to migrate into wound, and undifferentiated mesenchymal cells begin to transform into fibroblast.
Immediate to 3-5 days
:(Bleeding stops (hemostasis
a. Constriction of blood supply
b. Platelets start to dot
c. Formation of scab
:Inflammation
a. Opening of blood supply
b. Cleansing of wounds
CARDINAL SIGNS OF INFLAMMATION
Redness – rubor
Swelling – tumor
Warmth – color
Pain - dolor
Loss of function
/signs-of-inflammation-4580526_FINAL-5c6f21adc9e77c0001be5177.png)
Fibroplastic Stage
Strands of fibrin, from blood coagulation, crisscross wound to form a latticework on which fibroblasts can begin laying down ground substance & tropocollagen
Occurs 5 days to 3 weeks
:Granulation
a. New collagen is laid down
b. New capillaries fill defects
:Contraction
a. Wound edges pull together
: Epithelialization
a. Cells cross over the moist surface
b. Cell travel about 3mm from point of origin
Remodelling Stage
Final stage of wound repair
Continuous indefinitely, from 3 weeks to years
Also known as “WOUND MATURATION STAGE”
Previous randomly laid down collage are destroyed & replaced by new collagen fiber of better orientation to resist tensile forces of the wound
The final process, which begins near the end of fibroplasia & continues during the early portion of remodelling, is wound contraction
During wound contraction, the edges of the wound migrate toward each other
Wound strength never reaches 80-85% of the strength of un-injured tissue
As wound metabolism lessens, vascularity is decreased, which diminishes wound erythema
...ALWAYS REMEMBER
Inflammatory Stage | Fibroplastic Stage | Remodelling Stage |
3-5 days | 5 days to 3 weeks | 3 weeks to years |
FACTORS THAT IMPAIR WOUND HEALING
Foreign Material
Necrotic Tissue
Ischemia – restriction of blood and oxygen supply
Wound Tension
Foreign Material
"Is anything that the host organism’s immune system views as “non-self
This includes bacteria, dirt, suture material, etc
Bacteria can proliferate and cause an infection in which bacterial proteins that destroys host tissue are released
Non-bacteria foreign material acts as haven for bacteria by sheltering them from host defences & thus promoting infections
Foreign material is often antigenic & can stimulate chronic inflammatory reaction that decreases fibroplasia
Necrotic Tissue
Serves as a barrier to the ingrowth of reparative cells; prolonging the inflammatory stage since the white blood cells fail to remove the necrotic debris
Serves as a protected niche for bacteria
This frequently includes blood that collects in a wound (hematoma), where it can serve as an excellent nutrient source of bacteria
:Example of Necrotic Tissue secondary to extraction*

Ischemia
(Decreased blood supply & oxygen delivery to a wound.(Black or Bluish on color
Result to further tissue necrosis - Lessen delivery of antibodies, white blood cells, and antibiotics to the wound
:Caused by
Tight or incorrectly placed sutures
Improperly designed flap
Excessive external or internal pressure on a wound
Systemic hypotension
Peripheral vascular disease
Anemia
:Example of ischemia of oral tissue*

Wound Tension
Tension from sutures cause tissue strangulation, producing ischemia
If sutures are removed too early, wound under tension may re-open resulting to excessive scar formation and wound contraction
On the other hand, when sutures are left too long, the tract where the sutures ran will epithelize then leave a permanent disfiguring mark
HEALING BY PRIMARY INTENTION
Wound edges without tissue loss are places and stabilized in essentially the same anatomic position prior to injury
Wound repair occurs with minimal scar tissue
A theoretical ideal which is difficult to attain clinically
Generally used term to designate wounds which the edges are closely reapproximated
HEALING BY SECONDARY INTENTION
Implies that a gap between edges of incision or laceration or between bone or nerve ends after repair
Tissue loss prevents close approximation of wounds edges
Requires large amount of wound repair processes
Examples are extraction sockets, deep ulcers or large avulsive injuries
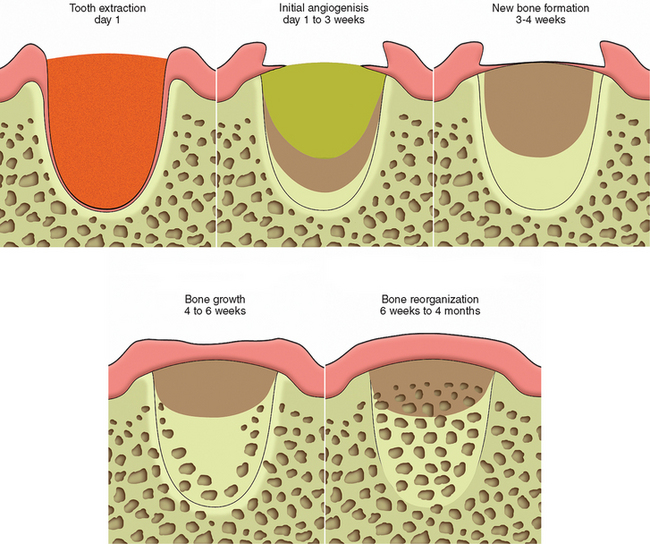
Healing of Extraction Sockets*
After extraction, the remaining empty socket consist of cortical bone (radiographically seen as the lamina dura) covered by torn periodontal ligaments, with a rim of epithelium (gingiva) at the coronal portion
The socket fills with blood, which coagulate and seals the sockets from the oral environment
:First week of healing
Inflammatory stage – White blood cells enter socket to remove contaminating bacterial & to begin break down of any debris left in the socket
Fibroplasia – ingrowth of fibroblasts and capillaries
Epithelium migrates down the socket wall until it reaches a level at which it contacts epithelium from the other side of the socket or when it encounters the bed of granulation tissue under the blood clot
Osteoclasts (Bone destroying cell) accumulate along crestal bone
:Second week of healing
Large amount of granulation tissue fill the socket
Osteoid deposition along the alveolar bone lining the socket
:Third-Fourth week of healing
Cortical bone continues to be resorbed from crest and walls of sockets
New trabecular bone is laid down across the socket
:4-6 Months
The cortical bone lining is fully resorbed, radiographically there is a complete loss of lamina dura
HEALING BY TERTIARY INTENTION
A term surgeon use to refer to wound healing through use of tissue grafts in large wounds
BONE HEALING
Bone heals by primary & secondary intention
If fracture ends are more than 1 mm or so apart, bone heals by secondary intention; wherein large amount of collagen must be laid down to bridge the bony gap
Fibroblasts and osteoblasts produce a lot of fibrous matrix such that healing tissue extends circumferentially beyond the free ends of the bone forming callus
Healing of bone by primary intentions occurs when bone is either incompletely fractured such that fracture ends does not become separated from each other,
Or when a surgeon closely re-approximates & rigidly stabilize fractured ends
In this case, little fibrous is produced & reossification of tissue within fracture area occurs quickly, with minimal callus formation
TWO FACTORS IMPORTANT TO PROPER BONE HEALING
Vascularity
If vascularity or oxygen supplies are sufficiently compromised, cartilage forms instead of bone
If either vascularity or oxygen supplies are poor, fibrous tissue does not chondrify or ossify
Immobility
Placing bone under continuous or repeated cycles of some tension stimulates continued osteoblastic bone formation
Bone is formed perpendicular to lines of tension to help withstand the forces placed on it
Excessive tension or torque placed on a healing fracture site produces mobility & compromises vascularity of the wound, promoting wound infection
IMPLANT OSTEOINTEGRATION
:Wound healing around dental implants; involves two basic factors
Healing of bone to the implant
Healing of alveolar soft tissue to the implant
HEALING OF THE BONE TO THE IMPLANT
This must occur before any soft tissue forms between the bone & the implant surfaces
:Four factors needed to achieve this
Short distance between implant & bone
Viable bone at or very near the surface of the bone along the implant
No movement of implant while bone is attaching to its surface
An implant surface free of contamination by organic or inorganic material. Including bacteria, oil, glove powder, foreign metals and foreign proteins
VIABLE BONY SURFACE ALONG THE IMPLANT
There should be minimized bone damage during site preparation to preserve the viability of the bone near implant surface
Much damage is caused by heat friction during cutting process
It is minimized by using sharp bone-cutting instruments, limiting cutting speeds to minimize frictional heat, & by keeping the bone cool with the irrigation during site preparation
Counter sinking implants & using low profile healing screws decrease chances of unwanted forces to be delivered to the implant
Covering the top of the implant during healing further protects it
?In implant, we use low-speed. Why*
Less torque to minimize damage to the bone & the healing capacity is intact
So that the drill keep on moving and penetrate the bone
FACIAL NEUROPATHY of TRAUMATIC ORIGIN
:The three branches of the trigeminal nerve injured most commonly
Inferior alveolar-mental nerve
Lingual nerve
Infraorbital nerve
types of nerve injuries
Neurapraxia
Axonotmesis
Neurotmesis
Neurapraxia
Least severe form of peripheral nerve injury
Contusion of a nerve in which continuity of the epineurial sheath and the axons is maintained
Blunt trauma or traction (e.g., stretching) of a nerve, inflammation around a nerve, or local ischemia of a nerve
No loss in axonal continuity, spontaneous full recovery of nerve function usually occurs in a few days or weeks
Axonotmesis
When the continuity of the axons but not the epineurial sheath is disrupted
Severe blunt trauma, nerve crushing, or extreme traction of a nerve
Because the epineural sheath is still intact, axonal regeneration can (but does not always) occur with a resolution of nerve dysfunction in 2 to 6 months
Neurotmesis
Most severe type of nerve injury
Complete loss of nerve continuity
Produced by badly displaced fractures, severance by bullets or knives during an assault, or by iatrogenic transection
Prognosis is poor except if the ends of the affected nerve have somehow been left in approximation and properly oriented
(NERVE HEALING (Two phases
Degeneration
a. Segmented demyelination
b. Wallerian degeneration
Regeneration
Segmented Demyelination
Myelin sheath is dissolved in isolated segments
This causes a slowing of conduction velocity and may prevent the transmission of some nerve impulses
:Symptoms
a. Paresthesia -a spontaneous and subjective altered sensation that a patient does not find painful
b. Dysesthesia -a spontaneous and subjective altered sensation that a patient finds uncomfortable
c. Hyperesthesia -excessive sensitivity of a nerve to stimulation
d. Hypoesthesia -decreased sensitivity of a nerve to stimulation
Occur after neurapraxic injuries or with vascular or connective tissue disorders*
Wallerian degeneration
Axons and myelin sheath of the nerve distal to the site of nerve trunk interruption' (away from the central nervous system) undergo disintegration in their entirety
Stops all nerve conduction distal to the proximal axonal stump
Occurs after nerve transection and other destructive processes that affect peripheral nerves
occurring after nerve trauma*
Regeneration
Normally the proximal nerve stump sends out a group of new fibers (the growth cone) that grow down the remnant Schwann cell tube
Growth progresses at a rate of 1 to 1 .5 mm/d and continues until the site innervated by the nerve is reached or growth is blocked by fibrous connective tissue or bone
Begin almost immediately after nerve injury*
Reference:
Lecture of Dr Reece Aldrin Valdez at national university college of dentistry- manila, philippines

برچسبها: Surgery
Anesthesis summery
A.Trigeminal nerve (Cranial nerve V) devision:
1.Ophthalmic (V1)
2.Maxillary (V2)
3.Mandibular (V3)
*sensory: To skin of the face, Nose & nasal cavity, Forehead, Temple, Teeth, Tongue, Palate .( involve V1,V2,V3)
*motor: To muscle of mastication & Anterior belly of digastric & Masseter.(only V3)
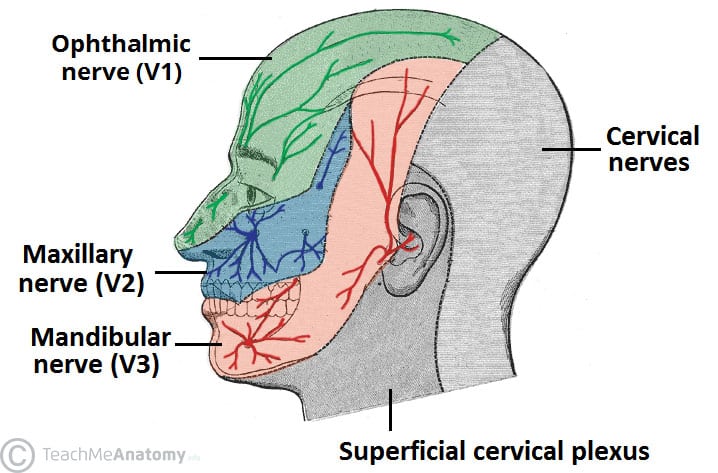
1. Ophthalmic (V1 ):

2. Maxillary (V2 ):
*Nasopalatine: Lower posterior nasal septum, Mucous membrane of anterior hard palate.
*Greater palatine: Mocous membrane of posterior hard palate.
*Lesser palatine: Soft palate of tonsils
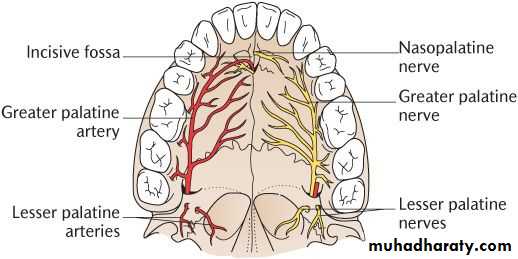
*Superior Alveolar Nerves:
Anterior Superior Alveolar Nerves (ASAN): Anterior teeth & Maxillary sinus
Middle Superior Alveolar Nerves (MSAN): Premolars & MB root of 1st molar & maxillary sinus
Posterior Superior Alveolar Nerves (PSAN): DB and palatal root of 1st molar , 2nd molar , 3rd molar , Maxillary sinus
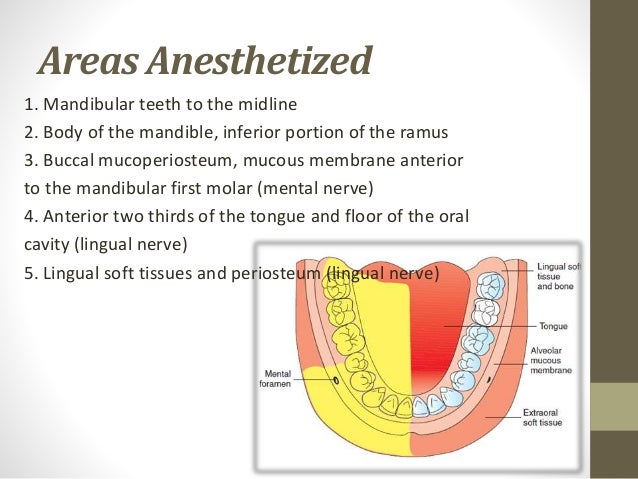
3. Mandibular (V3) :
*Lingual nerve: Anterior two third of the tongue, Lingual gland, Submandibular gland, Sublingual gland.
*Buccal nerve: Cheek, Buccal gingiva of lower molars
* Inferior Alveolar nerve (IAN): goes into the mandibular foramen
Dental nerve: Lower molars & Premolars
Mental nerve: Skin of lower lip & Chin (exits the mental foramen)
Incisive nerve: Lower Incisor & Canines
*Temporal nerve
*Lateral pterygoid nerve
*Medial pterygoid nerve
B.contraindicated:
*when there is infection or inflammation in the area of the injection site.
*when there is presence of pus because pus is Acidic and anesthesia is Base so its does not work & aside from that is too much painful, so aspirate &treat the pust before anesthesia.
*when the health of px is compromised.
C. Maximum Recomendation Dose:
*Maximum amount of carpules that can be use in a person at a time is 10 carpules.
*Using different types of carpules a person at a time can cause Anaphylactic shock.
*Choose the Anesthetic Drug base on px health condition; For example Never use Lidocaine for Asthma px causeit can increasing heart rate ,use Aritrocainre Or Never use Lidocaine for hyperthroid px cause it leads to anfractuous, use articaine.

D. Dosage Calculation:
*Formulla: Maximum Recomendation Dose ✖ Body Weight= Total ÷ Amount of lidocaine in 1 carpule
*Example: 20 kgr child can tolerate how many carpule of 2% lidocaine with vasoconstrictor?
For "Amount of lidocaine in 1 carpule" read the written information on the carpules that you bought (depends on the carpule brands)
Usually in 1 carpule 1.8 mL of 2% lidocaine is used.
2% lidocaine is equal to 20 mg/ml
So Amount of lidocaine in 1 carpule = 20 mg/mL ✖ 1.8 mL= 36 mg/carpule
Maximum Recomendation Dose ✖ Body Weight= Total ÷ Amount of lidocaine in 1 carpule
4.4 mg/kg ✖ 20 kg = 88 mg ÷ 36 mg/carpule = 2.4 carpules
It means to say for 20 kg child, you can use two & half carpules.
E. Local Anesthetic Drug Information:
*Most common used: 2% Lidocaine with vasoconsrictor 1:100 000 Epinephrine
*Epinephrine as vasoconstrictor increase pulse rate
*Before using the cartridge, sterile with 70% alcohol & wash with body temprature water.
*Place the carpule at Hot water for 5min for better control of the pain produced during the administration of dental anesthesia injection; because Heat can cause the lidocaine to be absorbed into your body faster .

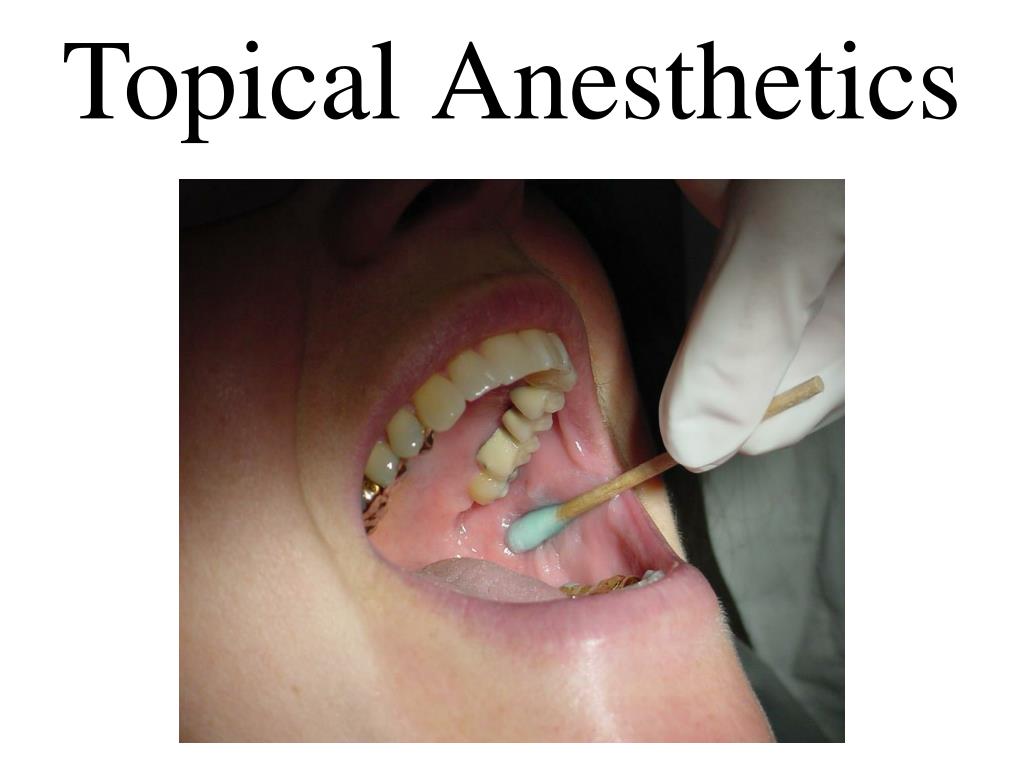
F. Topical anesthesitic:
Identify the landmarks by palpation & dry the area
Apply topical anesthetic Gel 20% Benzocaine. The Onset is 20 sec & recommended applying for 1-2 min & effecting time is 5-15 min.
Once the color of tissue change to white means " Blanching" that shows tissue numbness.
G. Needle:
As increasing # gauge we have decreasing of needle diameter
The most common gauges are 25, 27, and 30 gauge.
27 gauge, the smallest gauge -largest diameter) is highly suggested Because the diameter is small so it will not be painful for patient & easy aspiration but has enogh strength to penetrate the tissue without deflection.
Long needle is about 32 mm (1.5 inches) and the short needle is about 20 mm (1.0 inch).
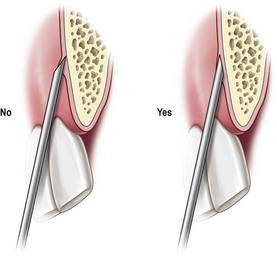
Bevel of the needle shoud face the cortical bone.
H. Aspiration & Deposite:
*Syringe should contain No air.
*Always make sure that you are heat the bone then, withdraw the needle 1mm
*Aspirate for 20 sec must be negativeTo make you sure that you will deposite in the nerve not in the blood vessels & if after aspiration you see the blood it means its positive & you must correct your needle position base on landmarkes
*After Aspiration, Deposite slowly in 60 sec ;To avoid pain and ulceration.
*Once you insert the needle ask the px to Inhale.
*Once you deposite the carpule ask the px to Exhale.
*Always Slowly remove the needle & palpate the area to help disturbution of anesthesia.
*Wait for 2-3 min to act.
H. Techniques:
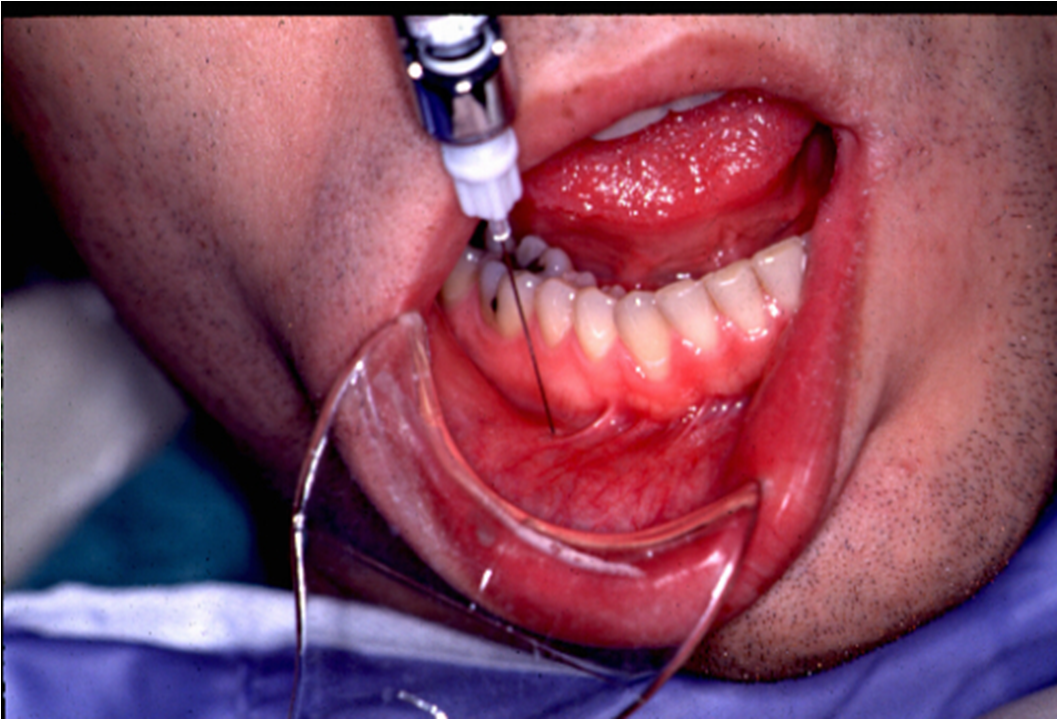
1. Inferior alveolar nerve block (IANB)
*Other name: Vazirani
*Numbness : Half of the mandible
*Once you need numbness of both side of mandible: Bilateral IANB
*Landmarkes & procedure:
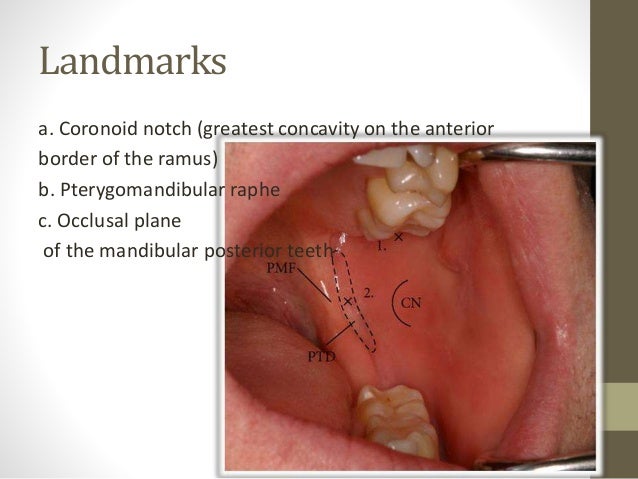
*Use Long needle 27 gauge
*Never use short needle for IAN BLOCK cause needle will break 
Needle should be at level of occlusal plane & between Lower 1st & 2nd PM .
For pediatric px needle should be above occlusal plane.

Slowly insert Half of the needle & heat the bone .
Change your neddle direction, Follow the central fossa of teeth & insert whole of the needle & Deposite the rest of the carpule.
*Example: Px came to your clinic for endo tx of tooth # 16. After Ian block & starting procedure, px is complaning of pain
1st complain : Proceed to Interligamentray anesthesia(Complement anesthesia for IAN) ; Bend the short 27 gauge needle by scoop technique & insert the needle 30 degree to interligument.
Anesthesia solution effects in interligament by passing PDL cell sheets(صفحات غربالی)

2nd complain: Intrapulpal anesthesia (secondary anesthesia); Bend the short 27 gauge needle by scoop technique & insert the needle 90 degree directly to the pulp.
*After IAN Block we proceed to Infiltration techmique for Reducing bleeding
2. Infiltration technique:
*Numbness: Soft tissue around the tooth & Dental plexus nerves
*Landmarkes & procedure:
On Labial or Buccal ,looks for Muccobual fold & Apex of root of the offending tooth.
On palatal, look for Gingival maring & Midline of the plate.
On Lingual, look for muco-lingual fold.
On Labial or Buccal, insert the needle 2mm away from the muccobucal fold at 45 degree till you heat the bone.
On palatal , insert the needle at 90 degree between Gingival maring & Midline of the plate.To achive this, the needle should derived from opposite side.
On Lingual, insert the needle above the muco-lingual fold to avoid dissemination of the solution into the floor of the mouth.

Deposite half of carpule on each side for 60 sec.
*Use 27 gauge short needle
3. Buccal nerve block
*Insert the needle parralel to occlusal plane, Distal to second molar.
*Use 27 gauge short needle with length of 20 mm (1.0 inch) .
*Deposit about 1 ml of solution around the inferior alveolar nerve.

4. Mental nerve block:
*Landmarkes:
Retract the cheek and lip & locate the junction of mandibular 1st &2nd premolars & down 1 cm inferior to the gum line (just medial to the midline pupil)
*Insert the needle Distal to second premolar.
*Use 27 gauge short needle.
*Deposit one third to one half of the cartridge.
*The difference between the mental nerve block & the incisive nerve block is that the incisive nerve block requires pressure to the mental foramen.
5. Incisive nerve block:
*This technique is painful and not used routinely especially for the pediatric patient
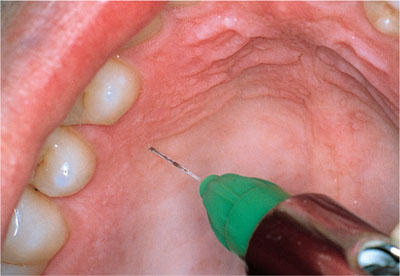
*Landmarkes & procedure:
Palatal mucosa just lateral to the incisive papilla (located in the midline behind the central incisors).
*Use 27 gauge short needle.
Insert the needle approaching incisive papilla at a 45 degree.
Place the cotton applicator directly onto the incisive papilla & Apply sufficient pressure so there is blanching.
Place the bevel of the needle against the blanched soft tissue at the injection site.
Apply enough pressure to slightly bow the needle.
Deposit a small amount of anesthetic; Straighten the needle and penetrate the tissue with the needle & Continue to apply pressure with the cotton applicator while injecting until bone is contacted (about 5mm).
Deposit no more than a ¼ cartridge.
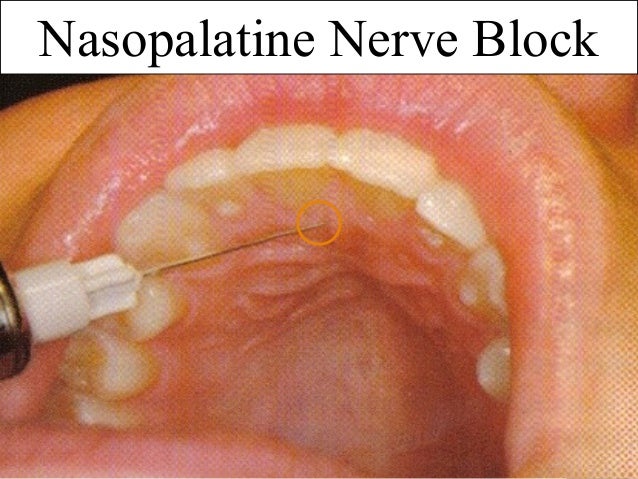
6. Greater palatine nerve block
* It is less traumatic than the nasopalatine nerve block because the palatal tissue in the area of the injection site is not as anchored to the underlying bone
*Landmarkes & procedure:
Maxillary first molar (or second primary molar in the primary dentition)

First Place a cotton swab at the junction of the hard palate and the maxillary alveolar process.
Apply pressure with the cotton swab while moving posteriorly.
The cotton swab on will fall into the depression created by the greater palatine foramen.
Move the cotton swabr posteriorly so it is directly over the greater palatine foramen and apply sufficient pressure to blanch the tissue for 30 seconds
Direct the syringe into the mouth from the opposite side of the mouth from the injection site at a 90 degree
Deposit a small volume of anesthetic( Straighten the needle and allow the needle to penetrate the mucosa, while depositing)
Slowly advance the needle approximately 8mm until palatine bone is contacted.
Deposite ¼ cartridge of anesthetic solution over 30 seconds.

Reference:
https://www.dentalcare.com/en-us
Lecture of Dr jimmy Aldecua & Dr Rea Corpuz at national university college of dentistry- manila, philippines
برچسبها: Surgery
CROWN LENGTHENING
Here I Want To Explain, Why Surgical Crown Lengthening After Extrusion Or Forced Eruption Is Much Better Rather Than Surgical Crown Lengthening Alone?
A.The Norrmal Anatomical Crown-Root Ration Ror an Average Central Incisor Is 11:14
B. Here Is a Example Of a Tooth that Fractured 3mm Beyond CEJ
C.Surgical Crown Lengthening ALONE Would Produce an Unstable & Unesthetic Crown-Root Ratio 14:11
D. Extrusion Followed By Crown Lengthening Produce a More Stable Crown-Root Ratio Of 11:11 With a More Esthetic and Normal Crown Length
برچسبها: Surgery
